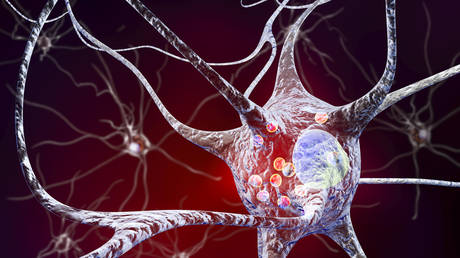
New Parkinson’s disease research indicates it may actually have two variants which start in different areas of the body. Scientists also worry the Covid-19 pandemic may lead to a major spike in the neurodegenerative disorder.
Parkinson’s is widely believed to be a singular, neurodegenerative disease which starts in the brain, but a new brain imaging study indicates it may actually be two simultaneous afflictions, one of which starts in the gut.
In some of the Parkinson’s patients observed, the disease started in their intestinal nervous system before traveling up into the brain.
“Until now, many people have viewed the disease as relatively homogeneous and defined it based on the classical movement disorders,” says neuroscientist Per Borghammer from Aarhus University in Denmark, adding that this new discovery will likely shift future research and treatment.
The small study of 37 participants between the ages of 50 and 85 had either been diagnosed with Parkinson’s or were considered “at-risk” and underwent Positron emission tomography (PET) and magnetic resonance imaging (MRI) scans.
In one rather odd twist in the study, researchers noted that a significant number of participants had a REM (Rapid Eye Movement) sleep disorder which resulted in them acting out their dreams.
This anomalous behavior tended to signal the Parkinson’s variant which begins in the gut. The scientists suspect this form then travels up to a part of the brain closely linked with REM sleep.
On the other hand, the brain-first Parkinson’s tends to originate in the substantia nigra part of the brain.
“We now have knowledge that offers hope for better and more targeted treatment of people who are affected by Parkinson’s disease in the future,” Borghammer added.
Borghammer proposes exploring whether body-first Parkinson’s can be treated differently, by using fecal transplants or other methods which target the gut biome, to try and stop the disease from spreading to the brain, where treatment is far more difficult to deliver and manage.
Sadly, in the brain-first variant, by the time symptoms begin to manifest themselves, cognitive degeneration is already somewhat advanced.
Meanwhile, researchers in Australia are sounding the alarm about a potential “silent third wave” of Covid-19-associated neurological conditions, including a possible spike in cases of Parkinson’s disease.
Long-term neurological damage was documented in the aftermath of the Spanish Flu last century in the form of encephalitis lethargica, a form of brain inflammation.
This, in turn, increased the risk of developing Parkinson’s by two to three times, and Covid-19 has already been linked to various forms and degrees of neurological damage.
“Although scientists are still learning how the SARS-CoV-2 virus is able to invade the brain and central nervous system, the fact that it’s getting in there is clear,” says neuroscientist Kevin Barnham from the Florey Institute of Neuroscience & Mental Health in Australia.
There is currently no direct evidence to suggest an impending wave of Parkinson’s, as it is too early to tell, but the underlying data suggests that such a “third wave” is worth taking seriously to avoid yet another unprecedented global public health disaster in the next few decades.
“Given that the world’s population has been hit again by a viral pandemic, it is very worrying indeed to consider the potential global increase of neurological diseases that could unfold down track. The world was caught off guard the first-time, but it doesn’t need to be again,” Barnham concluded.
Like this story? Share it with a friend!




